Table of Contents
The introduction of Amyloidosis:
Amyloidosis is a rare, progressive, and often fatal condition caused by the accumulation of abnormal proteins called amyloid in various organs and tissues throughout the body.
Amyloid is an abnormal protein usually produced by the body as a response to an injury or infection. In amyloidosis, the body has an excessive amount of amyloid, accumulating in the organs and tissues, causing damage and dysfunction.
The exact cause of amyloidosis is not known, but it has been linked to certain autoimmune diseases, genetic factors, and exposure to certain chemicals or toxins. Symptoms of amyloidosis vary greatly depending on the type and location of the amyloid deposits.
Common symptoms include fatigue, weight loss, swelling, and difficulty breathing. Other signs and symptoms may include an enlarged liver or spleen, changes in the skin, and nerve damage.
Diagnosis of amyloidosis is made through a combination of laboratory tests, imaging studies, and biopsies. Treatment of amyloidosis depends on the type and location of the deposits, but typically involves medication, lifestyle changes, and in some cases, stem cell transplantation.
Although amyloidosis is incurable, treatment can help slow the progression of the disease and improve quality of life.
The Definition of Amyloidosis:
Amyloidosis is a rare, serious, and potentially life-threatening disorder caused by the accumulation of an abnormal protein known as amyloid in various organs and tissues in the body.
Amyloid is an insoluble protein that accumulates in the body’s organs and tissues in the form of fibrils, which disrupt normal organ function. Amyloidosis is a systemic disorder, meaning it can affect multiple organs and systems in the body.
The most common type of amyloidosis is called primary amyloidosis, which is caused by the accumulation of amyloid deposits in the bone marrow. This type of amyloidosis is caused by the overproduction of a protein produced by plasma cells, which are a type of white blood cell.
Primary amyloidosis can lead to organ failure if not treated. Secondary amyloidosis is caused by the accumulation of amyloid deposits in other organs and tissues of the body due to another underlying medical condition, such as chronic infections, inflammatory diseases, or cancer.
Amyloidosis can lead to a wide range of symptoms, depending on the affected organs and tissues.

The Causes of Amyloidosis:
Amyloidosis is a rare disorder in which an abnormal protein called amyloid builds up in the body’s organs and tissues. The amyloid protein is made up of a variety of different proteins, each of which has a specific function in the body.
The primary cause of amyloidosis is an underlying medical condition or disease, such as multiple myeloma, lupus, rheumatoid arthritis, or certain types of infection.
These conditions can cause the body to produce abnormal proteins that can accumulate in organs and tissues. In some cases, the cause of amyloidosis is unknown. This is known as primary amyloidosis and is believed to be due to genetic mutations that cause abnormal proteins to be produced and accumulate in organs and tissues.
Other causes of amyloidosis include certain medications, such as certain antibiotics, chemotherapy drugs, and anti-inflammatory drugs. Certain toxins, such as lead and mercury, can also cause abnormal proteins to accumulate in the body.
In addition, certain inherited conditions, such as familial amyloid polyneuropathy and transthyretin amyloidosis, can cause amyloid proteins to accumulate in the body. Common symptoms can include fatigue, weight loss, and swelling in the legs.
The Risk Factors for Amyloidosis:
Amyloidosis is a rare and serious condition that occurs when an abnormal protein called amyloid builds up in one or more of your organs or tissues. The amyloid protein can damage the organs, disrupting their function.
Risk factors for amyloidosis include having certain conditions or diseases, being exposed to certain toxins, and having certain genetic mutations.
1. Conditions and Diseases: Certain long-term conditions and diseases can increase the risk of developing amyloidosis. These include autoimmune disorders such as rheumatoid arthritis or lupus, kidney disease, and certain types of cancer.
2. Exposure to Toxins: Certain toxins, such as heavy metals, can increase the risk of amyloidosis.
3. Genetic Mutations: Some people are born with a gene mutation that can increase their risk of amyloidosis. Such mutations can be inherited from a parent or can happen spontaneously.
4. Age: Amyloidosis can occur in people of any age, but it is more common in older people.
5. Gender: Amyloidosis is more common in men than in women.
6. Ethnicity: Amyloidosis is more common in certain ethnic groups, such as African Americans, Hispanics, and Asians.
7. Family History: People with a family history of amyloidosis are more likely to develop the condition.
If you have any of the risk factors listed above, it is important to talk to your doctor about your risk of amyloidosis and what steps you can take to reduce your risk.
The Symptoms of Amyloidosis:
Amyloidosis is a rare disease that occurs when abnormal proteins, called amyloid proteins, accumulate in one or more organs or tissues in the body. The amyloid proteins can form deposits in organs and tissues, causing them to become stiff and unable to function normally.
The symptoms of amyloidosis vary depending on the type and location of the amyloid deposits in the body. Common symptoms include:
• Fatigue
• Swelling in the abdomen, legs, or feet
• Shortness of breath
• Weight loss
• Weakness
• Numbness or tingling in the hands or feet
• Difficulty swallowing
• Muscle pain or cramps
• Abnormal heart rhythms
• Enlarged liver or spleen
• Enlarged tongue
• Skin changes, such as purplish patches
• Light-headedness or dizziness
• Loss of appetite
• Confusion or memory loss
• Difficulty sleeping
• Enlarged lymph nodes
• Blood in the urine
• Changes in skin color
• Anemia
• Decreased urine output
• Kidney failure
• Vision changes
• Hearing loss
• Neurological problems, such as numbness, weakness, or difficulty speaking If you experience any of these symptoms, it is important to seek medical attention right away to determine if you have amyloidosis.
Early diagnosis and treatment can help prevent further damage and potentially improve your prognosis.
The diagnosis of Amyloidosis:
Amyloidosis is a rare disorder caused by the buildup of abnormal proteins, called amyloid proteins, in the body’s organs and tissues. It can affect many different organs and systems of the body, and diagnosis can be difficult.
The diagnosis of amyloidosis begins with a physical exam and medical history. During the physical exam, a doctor may look for signs of organ damage or weakness.
For example, an enlarged heart or liver may be a sign of amyloidosis. The doctor may also order blood tests to look for the presence of amyloid proteins. These proteins are typically found at elevated levels in people with amyloidosis.
Other blood tests may be ordered to check for organ damage or to measure levels of certain hormones. Imaging tests such as X-rays, CT scans, MRIs, and ultrasounds may be used to look for signs of organ damage.
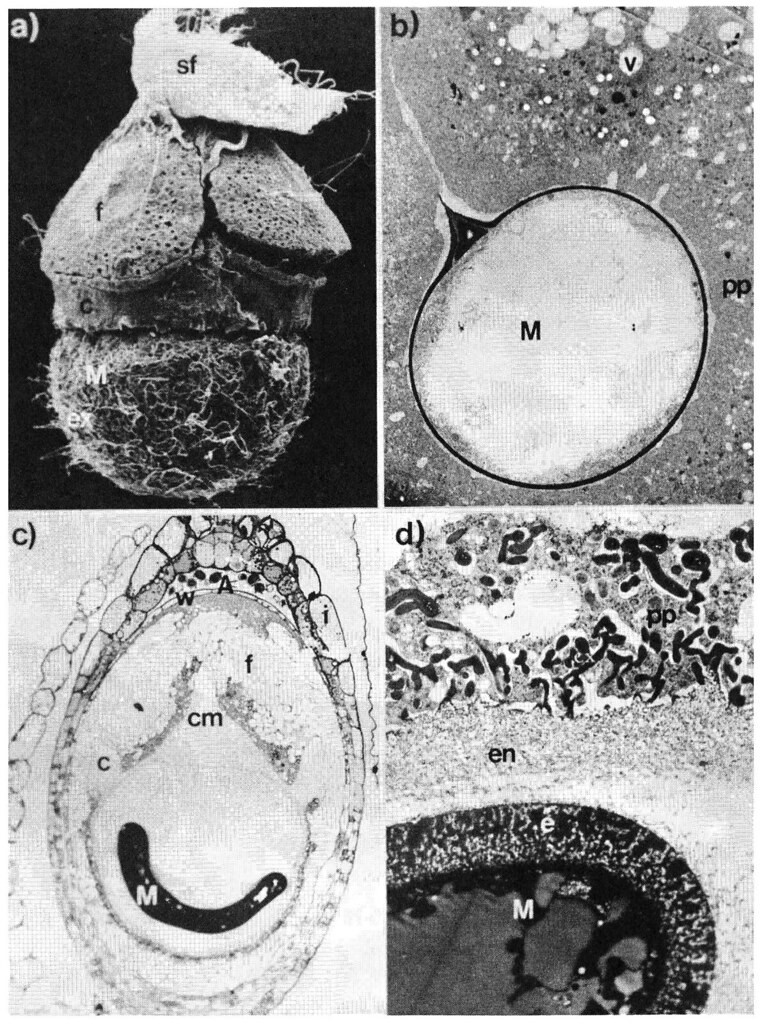
A biopsy of an affected organ may also be done. During a biopsy, a small piece of tissue is taken from the organ and analyzed under a microscope to look for abnormal deposits of amyloid proteins.
Once the diagnosis of amyloidosis is made, the doctor will determine the best treatment plan for the individual patient.
Treatment may involve medications to reduce symptoms, surgery to remove affected organs, or a combination of treatments.
The Treatment for Amyloidosis:
Amyloidosis is a rare, progressive, and potentially fatal condition in which proteins called amyloids to form deposits in tissues and organs, disrupting their normal functioning.
Treatment for amyloidosis varies depending on the type and severity of the condition. The main goal of treatment for amyloidosis is to reduce the amount of abnormal protein in the body and to prevent any further damage to the organs and tissues.
Treatment options may include:
• Corticosteroids: These medications can help reduce inflammation and help reduce the number of amyloid proteins in the body.
• Chemotherapy: This treatment involves the use of drugs to kill the abnormal cells producing the amyloid proteins.
• Immunomodulators: These medications can help reduce inflammation and can also help reduce the number of amyloid proteins in the body.
• Plasma exchange: This involves removing the fluid part of the blood (plasma) and replacing it with a solution to help reduce the number of amyloid proteins in the body.
• Bone marrow transplant: This procedure involves replacing the patient’s damaged bone marrow with healthy bone marrow from a donor. This can help reduce the number of amyloid proteins in the body.
Depending on the type and severity of amyloidosis, treatments may also include lifestyle changes such as quitting smoking, reducing stress, and exercising regularly. Some patients may also require surgery to remove affected organs or tissues.
In some cases, no treatment is needed and the condition will improve on its own. However, it is important to follow the doctor’s orders and seek medical help if any symptoms arise.
The Surgical Procedure for Amyloidosis:
Amyloidosis is a rare disorder in which a person’s organs and tissues are infiltrated with abnormal protein deposits. It can affect any organ in the body, but the most common organs affected are the heart, kidneys, and liver.
The surgical procedure for amyloidosis depends on the specific type of amyloidosis and the organs affected.
Heart: If the amyloidosis has affected the heart, the surgeon may perform a heart biopsy. During this procedure, a small sample of heart tissue is taken and examined under a microscope.
If the biopsy reveals the presence of amyloid deposits, the surgeon may recommend removing the affected tissue. This is done through a procedure called mastoidectomy, which involves removing the amyloid deposits from the heart using a special device.
Kidneys: If the amyloidosis has affected the kidneys, the surgeon may perform a kidney biopsy. During this procedure, a small sample of kidney tissue is taken and examined under a microscope.
If the biopsy reveals the presence of amyloid deposits, the surgeon may recommend removing the affected tissue. This is done through a procedure called a nephrectomy, which involves removing the amyloid deposits from the kidneys using a special device.
Liver: If the amyloidosis has affected the liver, the surgeon may perform a liver biopsy. During this procedure, a small sample of liver tissue is taken and examined under a microscope.
If the biopsy reveals the presence of amyloid deposits, the surgeon may recommend removing the affected . This is done through a procedure called hepatectomy, which involves removing the amyloid deposits from the liver using a special device.
The surgical procedures for amyloidosis are complex and require the expertise of a skilled surgeon. The procedures can be risky, and the success of the surgery depends on the type and extent of the amyloid deposits. Recovery time varies depending on the procedure, but it can take several weeks or months to fully recover.
The Prognosis and Outcomes of Amyloidosis:
Prognosis, The prognosis of amyloidosis, is highly variable and depends on the type of amyloidosis, the organs involved, and the patient’s overall health.
In general, the prognosis for patients with localized amyloidosis is better than for those with systemic amyloidosis. Localized amyloidosis is typically less severe and may be treatable with medications.
However, systemic amyloidosis is a progressive, potentially life-threatening condition, and the prognosis is often guarded. Outcomes The outcome of amyloidosis depends on the type, severity, and organs involved.
In general, patients with localized amyloidosis may have a more favorable outcome than those with systemic amyloidosis.
For localized amyloidosis, the goal of treatment is to control the progression of the disease and reduce symptoms.
Treatment often involves medications, lifestyle changes, and in some cases, surgery. For systemic amyloidosis, the goal of treatment is to reduce symptoms, slow the progression of the disease, and improve the patient’s quality of life.
Treatment options often include medications, chemotherapy, and stem cell transplantation. In some cases, amyloidosis may be successfully treated and the patient’s symptoms may go into remission.
However, amyloidosis is a progressive disease, and some patients may experience a decline in their condition despite treatment.
The Complications and Long-Term Effects of Amyloidosis:
Amyloidosis is a serious condition that occurs when abnormal proteins called amyloid deposits collect in the organs and tissues of the body. These deposits damage and interfere with the normal functioning of the organs and tissues, leading to a wide range of complications and long-term effects. Complications:
1. Kidney Damage: Amyloidosis can cause significant damage to the kidneys, leading to kidney failure and an increased risk of infection.
2. Heart Problems: Amyloid deposits can affect the heart and lead to abnormal heart rhythms, heart failure, and other serious heart problems.
3. Peripheral Neuropathy: Amyloid deposits can affect the nerves and cause pain, numbness, tingling, and other symptoms.
4. Skin Lesions: Some types of amyloidosis can lead to the development of skin lesions, which can be itchy or painful.
5. Gastrointestinal Problems: Amyloid deposits can interfere with the functioning of the gastrointestinal tract and lead to persistent diarrhea, nausea, and other digestive problems.
Long-Term Effects:
1. Organ Failure: Long-term amyloid deposits can cause serious damage to the organs and lead to organ failure and death.
2. Memory Loss: Long-term amyloid deposits can cause memory loss and cognitive impairment.
3. Fatigue: Long-term amyloid deposits can lead to extreme fatigue and decreased energy.
4. Anemia: Long-term amyloid deposits can lead to anemia and a decrease in the number of red blood cells.
5. Depression: People with amyloidosis are at an increased risk of developing depression due to the physical and emotional toll of the condition.
The Conclusion of Amyloidosis:
The conclusion of amyloidosis is that it is a complex and potentially fatal condition, but it can be successfully managed with careful management and early detection.
Early diagnosis and treatment of amyloidosis are essential to improve the patient’s prognosis. Treatment involves suppressing the underlying cause and eliminating the abnormal proteins.
Treatment options may include chemotherapy, radiation therapy, stem cell transplant, or other medications. It is important to understand that although there is no cure for Amyloidosis, it can be managed with proper treatment.
Finally, lifestyle changes, such as a healthy diet, regular exercise, and avoiding alcohol and tobacco use, can help reduce the risk of further complications.
The Reference to Amyloidosis:
Amyloidosis is a rare condition that occurs when a protein called amyloid builds up in one or more of your organs. It can affect any part of your body, but it commonly affects the heart, kidneys, liver, spleen, nervous system, and skin.
The most common type of amyloidosis, called AL amyloidosis, is caused by a clonal disorder, such as multiple myeloma or a lymphoproliferative disorder.
AL amyloidosis is a serious medical condition that can be life-threatening if not treated. Another type of amyloidosis is called AA amyloidosis. This type is caused by inflammation and is often seen in people with chronic inflammatory diseases, such as rheumatoid arthritis or inflammatory bowel disease.
The diagnosis of amyloidosis is based on a combination of physical exam findings, laboratory tests, and imaging studies. Laboratory tests include the serum free light chain test, which measures the amount of free light chains in the blood. Imaging studies may include a chest X-ray, CT scan, MRI, or echocardiogram.
Treatment of amyloidosis depends on the type and severity of the condition. Treatment may include medications to reduce inflammation, chemotherapy, radiation therapy, stem cell transplants, and other therapies. The goal of treatment is to reduce amyloid deposits and improve quality of life.
References:
1. Mayo Clinic. Amyloidosis. Available at: https://www.mayoclinic.org/diseases-conditions/amyloidosis/symptoms-causes/syc-20357484 (Accessed: 17th April 2021)
2. National Organization for Rare Disorders. Amyloidosis. Available at: https://rarediseases.org/rare-diseases/amyloidosis/ (Accessed: 17th April 2021)
3. Cleveland Clinic. Amyloidosis. Available at: https://my.clevelandclinic.org/health/diseases/17363-amyloidosis (Accessed: 17th April 2021)
4. American College of Rheumatology. Amyloidosis. Available at: https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Amyloidosis (Accessed: 17th April 2021)
5. National Heart, Lung, and Blood Institute. Amyloidosis. Available at: https://www.nhlbi.nih.gov/health-topics/amyloidosis (Accessed: 17th April 2021)
Also, read Magma geothermal energy source