Table of Contents
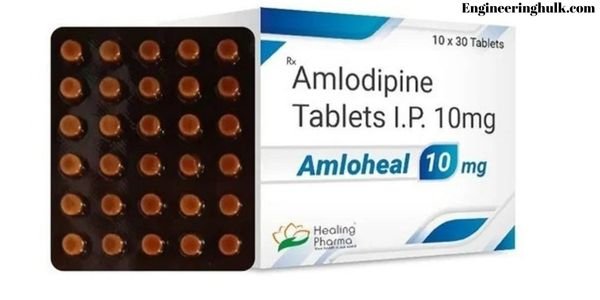
Introduction to Amlodipine
Amlodipine is a widely recognized medication in the medical community, primarily utilized for its effectiveness in treating high blood pressure (hypertension) and angina (chest pain). Classified under the category of calcium channel blockers, amlodipine functions by relaxing the blood vessels, allowing blood to flow more easily and thus reducing the heart’s workload. This mechanism not only helps in lowering blood pressure but also alleviates the symptoms of angina, contributing significantly to cardiovascular health management.
Commonly known by its brand names such as Norvasc, Katerzia, and Amvaz, amlodipine’s role in the treatment of cardiovascular conditions has made it a staple in therapeutic protocols. Given its critical function in dilating blood vessels and enhancing blood flow, amlodipine is often prescribed as part of a comprehensive treatment plan for individuals diagnosed with hypertension or chronic stable angina. The medication’s ability to improve blood circulation and reduce the risk of heart-related complications underscores its importance in contemporary medical practice.
The significance of amlodipine extends beyond its primary applications. By effectively managing high blood pressure, the medication helps in preventing more severe health issues such as stroke, heart attack, and kidney problems. Its contribution to reducing the strain on the heart and blood vessels makes it an indispensable tool in the arsenal against cardiovascular diseases. As healthcare professionals continue to advocate for the management of blood pressure and heart conditions, the utilization of amlodipine remains critical in promoting long-term health outcomes.
Amlodipine is a medication classified as a calcium channel blocker, a category of drugs that play a crucial role in cardiovascular health by modulating the movement of calcium ions across cellular membranes. Calcium ions are essential for muscle contractions, including those of the heart and blood vessels. By inhibiting the influx of calcium into the muscle cells of the heart and the arterial walls, amlodipine induces a relaxation of these muscles. This relaxation results in the dilation, or widening, of the blood vessels, a process known as vasodilation.
When blood vessels dilate, resistance to blood flow decreases, which enhances the overall circulation of blood throughout the body. This improvement in blood flow reduces the effort required by the heart to pump blood, thereby lowering the workload on the heart. Consequently, the heart can function more efficiently, which is particularly beneficial in conditions where the heart’s workload is increased, such as hypertension (high blood pressure) and angina (chest pain due to reduced blood flow to the heart muscle).
The primary physiological effect of amlodipine on the cardiovascular system is the reduction of blood pressure. By decreasing vascular resistance, amlodipine helps to lower systolic and diastolic blood pressure, which is critical in managing hypertension. Additionally, the reduction in the heart’s workload and the improvement in blood flow can alleviate symptoms of angina, providing significant relief to individuals suffering from this condition. Furthermore, the medication’s ability to prevent the constriction of blood vessels can also aid in the prevention of certain types of cardiovascular events, such as strokes and heart attacks.
Overall, amlodipine’s mechanism of action as a calcium channel blocker makes it an essential medication in the treatment of various cardiovascular conditions. Its role in promoting vasodilation, improving blood flow, and reducing cardiac workload highlights its importance in managing hypertension and angina, ultimately contributing to better cardiovascular health and patient outcomes.
Uses and Indications
For angina, amlodipine helps by improving blood flow to the heart muscle, which reduces the occurrence of chest pain. It is particularly effective in cases of chronic stable angina and Prinzmetal’s angina, where it helps to prevent the spasms of the coronary arteries. Clinical studies have shown that amlodipine can significantly lower the frequency and severity of angina attacks, improving the quality of life for patients.
Beyond its primary uses, amlodipine is sometimes prescribed off-label for other conditions. For instance, it is beneficial in the treatment of Raynaud’s phenomenon, a condition characterized by poor blood flow to the extremities. Additionally, some studies suggest that amlodipine may have a role in treating certain types of heart failure, particularly when combined with other medications. However, these uses are less common and typically considered when patients do not respond well to first-line treatments.
Statistical data further validates the effectiveness of amlodipine in these conditions. According to a study published in the Journal of the American College of Cardiology, patients taking amlodipine for hypertension experienced a significant reduction in systolic and diastolic blood pressure. Similarly, research in the American Heart Journal indicated a notable decrease in the frequency of angina episodes among those treated with amlodipine.
Overall, amlodipine’s versatility in treating hypertension and angina, along with its potential off-label benefits, makes it a valuable medication in the cardiovascular therapeutic arsenal. Its proven efficacy and safety profile continue to support its widespread use in clinical practice.
Dosage and Administration
The typical dosage recommendations vary based on the condition being treated and the patient’s age and overall health. For adults, the initial dose usually starts at 5 mg once daily, which can be adjusted up to a maximum of 10 mg per day, depending on the patient’s response to the treatment. For children aged 6 to 17 years, the starting dose is generally 2.5 mg to 5 mg once daily.
It is essential to adhere strictly to the prescribed dosage and administration guidelines provided by a healthcare professional. Amlodipine can be taken with or without food, making it a convenient option for many patients. However, consistency in the timing of the medication administration is crucial for maintaining stable drug levels in the body. Therefore, patients are advised to take amlodipine at the same time each day.
Patients should not adjust their dose without consulting their healthcare provider. Any changes in dosage should be based on a doctor’s evaluation of the patient’s response to the medication and any side effects experienced. Abrupt changes in dosage can lead to undesirable health consequences, such as an increased risk of adverse reactions or diminished therapeutic effects.
Moreover, it is important to follow the doctor’s advice regarding the use of amlodipine and to report any unusual symptoms or side effects promptly. Adherence to these guidelines ensures optimal management of the patient’s condition and minimizes the risk of complications associated with improper use of the medication.
Benefits of Amlodipine
Amlodipine, a widely prescribed medication, is renowned for its efficacy in managing various cardiovascular conditions. One of its primary benefits is its ability to significantly lower blood pressure. By relaxing the blood vessels, amlodipine enhances blood flow, thereby reducing the strain on the heart. This mechanism not only aids in achieving optimal blood pressure levels but also plays a crucial role in preventing hypertension-related complications.
Another notable advantage of amlodipine is its effectiveness in reducing the risk of stroke and heart attack. Clinical studies have consistently demonstrated that patients on amlodipine therapy experience a marked decrease in the incidence of these life-threatening events. The medication’s capacity to maintain stable blood pressure levels ensures that the cardiovascular system operates more efficiently, thereby minimizing the likelihood of abrupt cardiac events.
Additionally, amlodipine is highly beneficial in alleviating chest pain associated with angina. By improving blood supply to the heart muscles, helps in preventing angina attacks, thus allowing patients to lead a more active and pain-free life. Many patients have reported a significant improvement in their quality of life due to the reduction in frequency and intensity of angina episodes.
Long-term benefits of amlodipine have also been observed in various clinical trials. Studies indicate that consistent use of the medication results in sustained blood pressure control, which is essential for long-term cardiovascular health. Moreover, patients have reported fewer hospital visits and a reduction in the need for emergency medical interventions.
Patient testimonials further highlight the positive impact of amlodipine. For instance, John, a 58-year-old patient, shared that after starting amlodipine, his blood pressure normalized, and he experienced fewer angina attacks, significantly enhancing his daily functioning. Such real-world experiences underscore the transformative potential of amlodipine in managing cardiovascular conditions effectively.
Side Effects and Risks
It comes with a range of potential side effects that users should be aware of. Common side effects include swelling, particularly in the ankles and feet, which is often referred to as peripheral edema. This can be accompanied by a sensation of dizziness, especially when standing up quickly, due to its blood pressure-lowering effects. Patients might also experience fatigue, feeling unusually tired or weak, which can impact daily activities.
While these side effects are relatively common and generally manageable, there are also rare but serious side effects that warrant immediate medical attention. Severe allergic reactions to amlodipine, although uncommon, can manifest as difficulty breathing, swelling of the face, lips, tongue, or throat, and severe skin rashes. These symptoms require urgent medical intervention. Additionally, some patients might experience liver problems, indicated by yellowing of the skin or eyes (jaundice), dark urine, or severe abdominal pain. Worsening chest pain or new onset of chest pain (angina) after starting amlodipine is another critical side effect that should not be ignored.
Patients must consult their healthcare provider if they experience any side effects, whether common or rare. A healthcare professional can guide managing side effects, adjusting dosages, or considering alternative treatments if necessary. Self-monitoring and prompt reporting of adverse effects play a significant role in the safe and effective use of amlodipine. By maintaining open communication with their healthcare provider, patients can ensure that their treatment regimen is both safe and effective, minimizing the risks associated with this medication.
When taking amlodipine, it is crucial to be aware of potential interactions with other medications. Amlodipine, a calcium channel blocker, is commonly prescribed to manage high blood pressure and angina. However, its effectiveness and safety can be compromised by interactions with other drugs, necessitating careful management and communication with healthcare providers.
Blood Pressure Medications
Combining amlodipine with other blood pressure medications can lead to significant changes in blood pressure control. For instance, when used alongside beta-blockers, ACE inhibitors, or diuretics, there is a potential for additive effects, which may result in an excessive drop in blood pressure. This condition, known as hypotension, can cause symptoms like dizziness, fainting, or even shock in severe cases. Therefore, monitoring blood pressure closely and adjusting dosages accordingly is essential when these medications are co-administered.
Heart Medications
Patients taking other heart medications, such as digoxin or antiarrhythmics, should exercise caution. Amlodipine may increase the levels of digoxin in the blood, potentially leading to toxicity. Symptoms of digoxin toxicity include nausea, vomiting, visual disturbances, and severe cardiac arrhythmias. Similarly, interactions with antiarrhythmics can exacerbate side effects or alter the intended therapeutic effects. Healthcare providers often need to adjust dosages or select alternative treatments to mitigate these risks.
Over-the-counter drugs and Supplements
Over-the-counter drugs and supplements can also interact with amlodipine. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, may reduce the antihypertensive effects of amlodipine, making blood pressure more difficult to control. Additionally, certain herbal supplements like St. John’s Wort can alter the metabolism of amlodipine, leading to either increased side effects or reduced efficacy. Patients need to disclose all over-the-counter medications and supplements to their healthcare provider to ensure the safe and effective use of amlodipine.
In light of these potential interactions, patients should always inform their healthcare provider about all medications and supplements they are taking. This practice enables the provider to make informed decisions, adjust dosages, and monitor for adverse effects, ensuring the optimal therapeutic outcome while minimizing risks.
Precautions and Warnings
When considering the use of amlodipine, it is crucial to be aware of specific precautions and warnings to ensure safe and effective treatment. Amlodipine, a calcium channel blocker, is commonly prescribed for managing high blood pressure and angina. However, its use demands careful attention to individual health conditions and circumstances.
Pregnant and breastfeeding women should exercise caution with amlodipine. Although animal studies have not demonstrated significant risk, there is a lack of comprehensive human studies. Thus, it is recommended to use amlodipine during pregnancy only if the potential benefits justify the potential risks to the fetus. Breastfeeding mothers should consult their healthcare provider to weigh the benefits and potential risks before starting amlodipine, as it is unknown whether this medication passes into breast milk.
Patients with liver disease must be particularly cautious, as amlodipine is metabolized in the liver. Liver impairment could lead to elevated levels of the drug in the bloodstream, increasing the risk of side effects. It may be necessary to adjust the dosage or monitor liver function regularly to prevent complications. Similarly, individuals with heart disease, especially those with severe aortic stenosis or a recent history of heart attack, should use amlodipine with caution due to the potential for exacerbating heart-related issues.
Elderly patients are often more sensitive to the effects of medications, including amlodipine. Age-related changes in drug metabolism and an increased likelihood of comorbid conditions necessitate careful dosage adjustments and close monitoring. The potential for dizziness, a common side effect, is particularly concerning in this age group due to the increased risk of falls.
Regular monitoring and follow-up appointments with a healthcare provider are essential when using amlodipine. These check-ups help ensure the drug is working effectively and mitigate any adverse effects. Blood pressure should be regularly monitored, and any unusual symptoms should be promptly reported to a healthcare professional. This proactive approach helps in managing the condition effectively while minimizing potential risks associated with amlodipine use.
Also, read Metronidazole: Uses, Benefits, Side Effects, and More